Case studies
Electronic Health Records Shared, Nephrons Spared at Bradford
Share this on – Facebook / Twitter / Linked In

Primary care electronic health records (EHRs) are often inaccessible to secondary care staff. More traditional means of communication between community and hospital teams are generally inefficient for health services. Primary care practices in Bradford use a single centralised IT system (SystmOne®) that allows the sharing of detailed electronic health records by groups of healthcare professionals in various care settings. We have developed innovative EHR functionality to harness the power of record sharing and improve the quality of care of patients with both acute and chronic kidney disease.
- The CKD Electronic Consultation (e-consultation) Service
Primary care teams have assumed greater responsibility for the management of CKD in recognition of the need to identify the condition at an early stage and then intervene to slow disease progression and reduce cardiovascular morbidity and mortality. The CKD electronic consultation (e-consultation) service allows GPs to share a patient’s EHR with a renal specialist after first obtaining and recording the patient’s verbal consent. The specialist can view important clinical details such as patient comorbidities, medication history, lifestyle factors, previous communications from other specialists, reports of previous imaging and a chronological display of selected numerical data (blood pressure, estimated glomerular filtration rate, blood biochemistry and urinalysis), and then decide whether a patient should be referred to clinic or undergo tests or interventions in primary care.
The service is presented to GPs as a way of either obtaining specific management advice or requesting virtual review of patients with a borderline indication (as defined in local e-guidance) for making a hospital nephrology clinic referral. Such patients no longer need to wait several weeks for a hospital appointment and their care often remains in the hands of the primary care team.
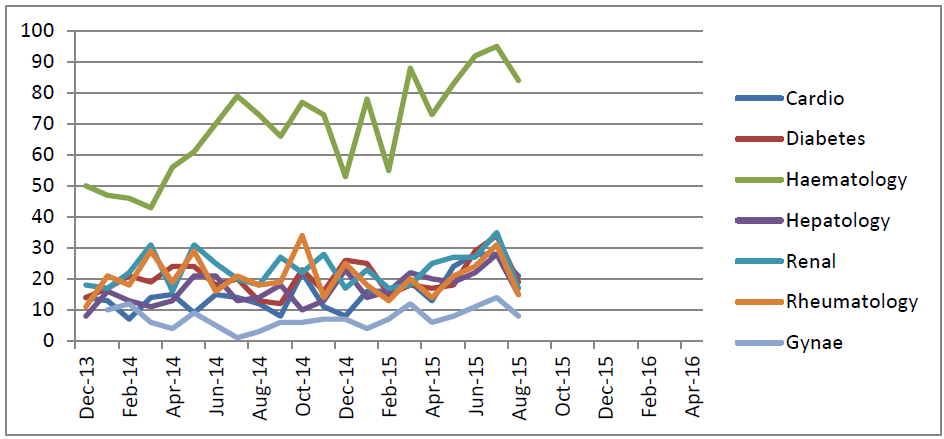
E-consultation helps to strengthen working relationships between GPs and hospital specialists, increase GP confidence in managing CKD in the community, and reduce transport and other environmental costs. Patients are generally very willing to consent to the viewing of their EHR by a renal specialist. A service evaluation has confirmed that renal function remains stable in patients who continue to be managed in primary care. [1] The e-consultation service is now available to other chronic disease specialties (activity graph attached) and other Trusts.
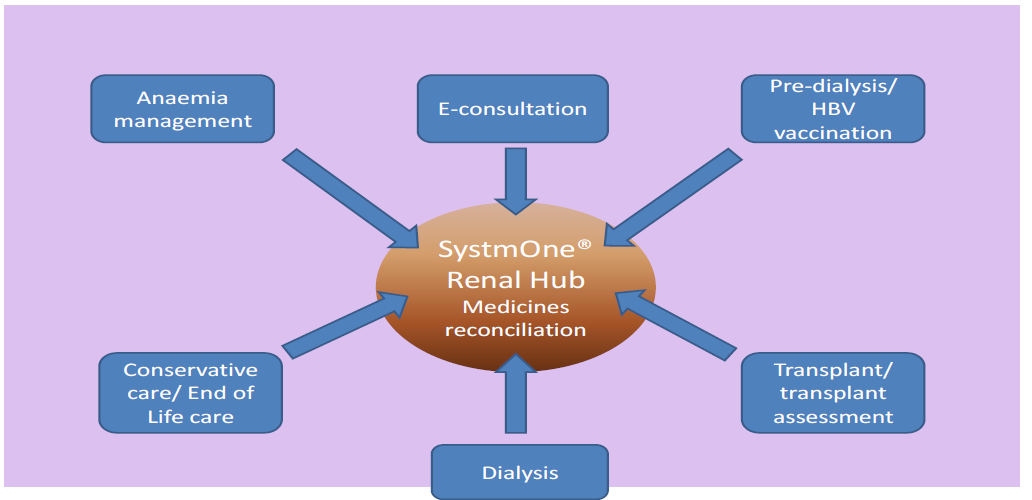
- The Bradford Renal Unit Hub
Following the experience of e-consultation, we decided to set up a Renal Unit Hub within our primary care EHR to facilitate two-way sharing of information with primary care for our RRT/ low clearance population, thereby reducing duplication of tests and supporting medicines reconciliation and care pathways that are shared with GPs (such as medicines reconciliation, anaemia management, hepatitis B vaccination, dialysis and transplant updates and a single shared conservative care pathway). This reduces administration time for the renal MDT and improves patient safety through more effective communication. [2]
- A Sick Day Alert for Healthcare Professionals
A more timely recognition of incipient AKI in the community and the acute admission areas of our hospital is likely to have a significant impact on AKI incidence and severity, with an associated reduction in hospital admission rates, patient morbidity and patient mortality.
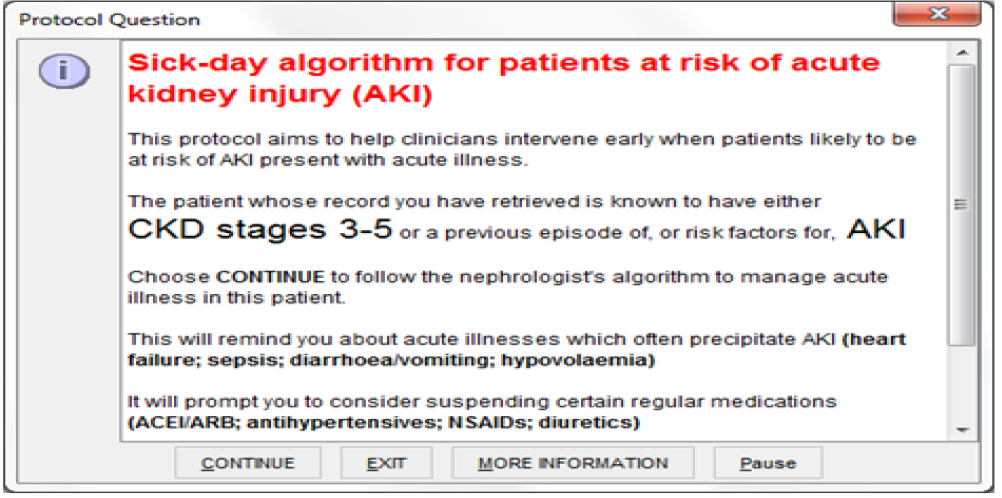
We have developed an automated Sick Day Alert within the SystmOne EHR for patients with coded risk factors for AKI, including advanced age, patients with chronic conditions such as diabetes, chronic kidney disease, congestive cardiac failure and chronic liver disease, and those who are established on medications that may need to be suspended at the time of acute illness.
The ‘Sick Day Alert’ is a simple reminder for healthcare staff in primary and secondary care to review medication and consider reversible elements such as dehydration and sepsis. The alert appears at the time of accessing a patient’s EHR in all healthcare settings including home, GP surgeries, Out-of-Hours facilities and the hospital front door. The first page of the alert in its current form is shown below.
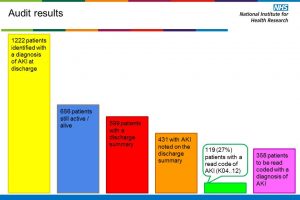
- A Care Bundle to Support the Release of the National AKI Detection Algorithm
In addition to promoting AKI prevention, AKI detection in primary care will soon be supported by the national laboratory AKI detection algorithm, now mandated by NHS England as part of the Think Kidneys programme. AKI management advice in our Trust has been formatted as a care bundle, as part of a multicentre Health Foundation Tackling AKI Scaling Up project led by Dr Nick Selby and colleagues in Derby. A modified care bundle is being developed for inclusion in the primary care EHR (current hospital version as below).
References
- Stoves J, Connolly J, Cheung CK, Grange A, Rhodes P, O’Donoghue D, Wright J. Electronic consultation as an alternative to hospital referral for patients with chronic kidney disease: a novel application for networked electronic health records to improve the accessibility and efficiency of healthcare. Quality & Safety in Health Care 2010, 19(5):e54
- John Stoves, Annie Wong, Ayesha Orlando, Vicki Hipkiss, Jeanette Middleton, Essi Lampinen, Tony Coman, Gary Carlisle, Wendy Green and John Connolly. Electronic patient record sharing between primary and secondary care to support renal pathways. British Journal of Renal Medicine 2014;19:12-14
For further information please contact Dr John Stoves John.Stoves@bthft.nhs.uk and Dr John Connolly john.connolly@tpp-uk.com
NB Think Kidneys has a statement on sick day rules /guidance here
Case studies