Case studies
Working Together in Southern Derbyshire to Improve the Care of People at Risk of or With Acute Kidney Injury
Share this on – Facebook / Twitter / Linked In

This case study provides information about the two year project to develop the local response to AKI with the overall aim of improving outcomes for patients.
Two perspectives are represented here – NHS Southern Derbyshire Clinical Commissioning Group and Derby Teaching Hospitals NHS Foundation Trust. Contact details are included for anyone wishing to know more.
Commissioning for quality improvement for people at risk of, or who have had, Acute Kidney Injury in NHS Southern Derbyshire CCG (SDCCG)
In October 2013, NHS England’s National Clinical Director for Renal launched a national programme of work to look at improving the safety, outcomes and experience of people at risk of, or who had suffered an episode of acute kidney injury (AKI). This was in parallel with NHS Commissioning Assembly also doing some work around Commissioning and AKI. This was in response to the growing global body of evidence that supports the low awareness, high mortality and morbidity as well as the high cost to the patient and healthcare services of AKI. The national programme comprised six workstreams, each working on different elements of quality improvement relating to AKI. One of the workstreams was to focus its effort on the identification of commissioning levers to drive improvements in the prevention, detection, management and treatment of AKI.
This paper outlines how Southern Derbyshire CCG got involved in this work over the course of a year and how it will take the work forward into a second year. As results emerge from the various workstreams further communications will follow. The following outlines activities in date order
October 2013 – Initial informal support and fact finding
Initial discussions were positive and support for the CCG to be involved was gained from the CCG Director Lead for Quality and Patient Safety (who is also the Chief Nurse with clinical knowledge and an appreciation of risks), the CCG Chief Officer and CCG Clinical Lead.
Informal discussions took place over the next few weeks with senior people across the CCG to highlight the issues and obtain support. We involved key people working in medicines management, primary care and secondary care commissioning and contracts teams in the discussions. This varied stakeholder group was identified to help scope the work and ensure key people were engaged at an early stage to bring expertise and commitment.
December 2013 – Formal wider support and discussion
The programme needed to be supported by the Clinical Commissioning Committee, which includes clinicians from the CCG as well as senior management representatives. A presentation proposed developing the work that would consider commissioning levers that could be implemented in the healthcare community. The aim of this work would be to raise awareness of the issues around the management of AKI and to improve patient safety, experience and outcomes for people at risk of, or who had experienced an episode of AKI.
The presentation was given by one of the Heads of Clinical Quality and also a Consultant Nephrologist, both of whom were directly linked into the Think Kidneys National Programme for AKI and therefore had good understanding of the issues involved. The Chief Nurse also provided support. At this time, so early on in the development of the National Programme, there were no concrete plans in terms of exactly what would be done as this was something new that had never been done before. However we were able to outline that the work would include the development of CQUIN activity in secondary care, commissioning activity in primary care and other aspects of healthcare over the next 3 years. It was anticipated work would be led by the CCG with a local steering group comprising stakeholders from the CCG, secondary care, and primary care and care homes.
We recognised a need to regularly report progress on the work to the CCG Quality Assurance Committee. We also knew that when commissioning proposals were developed and became more concrete, that they would be brought back to the Clinical Commissioning Committee for full approval. This gave the necessary assurances to the Committee that a governance framework would be in place and adhered to.
Full support was given to take forward the project.
It was important to ensure that the CCG executive recognised that the AKI work was aligned with the CCG’s strategic agenda, its work on patient safety, and was part of the national agenda as well as innovative in its approach and that positive outcomes would be delivered. Sign-off by the Clinical Commissioning Committee and Director support were two key requirements to enable the work to begin and continue.
December 2013 – Convening a steering group with the right people to maintain momentum
Members of the planned steering group were contacted individually by telephone and invited to an initial meeting. If they agreed to be involved an email message was then sent which provided information highlighting the issues and plans for the future. This ensured everyone received the same information.
Steering group members included
- CCG members
- heads of clinical quality for primary, secondary care and care homes
- medicines management – primary and secondary care
- primary and secondary care commissioning teams
- patient representation from patient who experienced AKI
- primary care clinicians – both GPs and practice nurses
- secondary care clinicians – nephrologists, cardiologist and emergency medicine clinician
- regional commissioning representatives and
- a representative from NHS England
We agreed that if further people were needed on the steering group they could be co-opted as necessary. The Deputy Chief Nurse/Head of Clinical Quality Primary Care) was named as the project lead for the work to ensure continuity, communication and momentum of the work. The Chief Nurse and Director of Quality for the CCG was named as the chair of the steering group. It was felt important to have a director in the chair as it would be recognised that senior leadership would bring direction and control to the project.
January 2014 – Gaining momentum, providing information and learning about the landscape and priorities
Enthusiasm for the start of the project drove us to hold the first steering group meeting quickly so that we could capitalise on the momentum that was building for the initiative. A presentation outlined what the National Programme was aiming to achieve and the importance of the commissioning perspective. We also knew it was important for us all to understand the priorities of everyone present and those they represented and the commissioning timescales. From the intelligence we were able to gather an initial work plan could be developed.
We agreed meetings should be held monthly despite how busy everyone was so that we could maintain momentum. Minutes were taken and circulated along with an updated work plan and any other papers for future discussion. Communication across the steering group was clear and we quickly started to see progress. We agreed that the commissioning timescales for secondary care CQUINs made it a priority area for our work.
A ‘Think Kidneys’ National Programme meeting was held which SDCCG steering group members attended. The meeting considered work priorities for the programme. Following this a draft CQUIN was brought to SDCCG and this was discussed and changed accordingly to meet local requirements. It was then taken to the Clinical Commissioning Committee for approval.
February 2014 – Quick progress
The secondary care two-part CQUIN was drafted and sent out for discussion and negotiation. A key incentive was set by the CCG as the AKI CQUIN was attached to a significant amount of money, making it an important driver for the hospital trust.
Next two months – Communication, raising awareness and plans for primary care
Over the next couple of months, the secondary care CQUIN was developed and agreed and processes to raise awareness were put in place. This included data collection to support the CQUIN.
Plans were also made to develop a Locally Commissioned Service Framework for primary care which would include AKI. However it was felt locally, that it was important to initially raise awareness and education amongst primary care clinicians (doctors and nurses) about AKI before any other changes were introduced. We agreed therefore that the first initial commissioning lever related to primary care and AKI would focus on this. This approach was supported following discussion at a National meeting.
A two-part Locally Commissioned Service (LCS) was written and taken to the Clinical Commissioning Committee for approval. The Head of Primary Care Commissioning and the Head of Clinical Quality for Primary Care visited individual clinical locality groups to introduce and discuss the concept. The LCS was also critiqued by a virtual group of primary care clinicians and practice staff before being taken to the Clinical Commissioning Committee. Everyone’s comments were taken into consideration.
This LCS was due to be implemented over an 18 month period from October 2014. The first part was to be implemented by April 2015 and the second part to run from April 2015 to March 2016. This was approved, though we recognised implementation would need support and on-going discussion to get this adopted in practices but to date most practices have taken part in the LCS.
Communication and governance
Communication within the SDCCG local steering group was on-going and all meeting minutes and papers were available to be viewed on the CCG intranet.
Reports were provided quarterly to the CCG Quality Assurance Committee and at the same time, progress on the programme was reported in the acute hospital trust through their quality structure.
A quarterly progress update was also provided to the Think Kidneys Programme Board, the Commissioning Assembly and NHS England. This ensured that all stakeholders interested in the programme were aware of activities and updated on progress overall.
As plans progressed, communications were also sent out via primary care newsletters and monthly CCG bulletins to start the flow of bite sized amounts of information and to encourage discussion and engagement. Face to face engagement was also important and we felt it was good to meet clinicians and managers in their environments (both in secondary and primary care) to get their views and ensure their perspectives were considered.
Communication was essential in the early stages, as this led to wider communication and awareness raising, not just with clinicians but also with the wider public. However the Think Kidneys national programme is ensuring work from all of the workstreams was communicated and we will be working with them to promote and spread the learning and impact of our work.
In summary
Within the first nine months of the project going live, we had implemented a secondary care CQUIN and the supporting mechanisms required. We had written the LCS and were ready to implement it in Primary Care. We also had plans to consider the development of a CQUIN for AKI for care homes.
In the future our work will focus on evaluating the impact of the new mechanisms and developing them further in response to what we learn and observe. But we recognise we cannot do this unless change happens. The progress we have made at such a fast pace would not have been possible without strong leadership, and highly motivated steering group members from the right areas. Success was the result of the fact that we shared a vision for the programme, and a commitment to innovation and good communication. We had support from senior CCG members, senior hospital trust members and the Think Kidneys Programme Board.
These are early days and the long-term success has yet to be identified and acknowledged. But here in SDCCG we have got off to a positive start in attempting to improve the safety, experience and outcomes of those who have experienced or are at risk of developing acute kidney injury.
If you would like to discuss our work, or would like further information please contact
Lynn Woods – lynn.woods@southernderbyshireccg.nhs.uk, Chief Nurse and Director of Quality, NHS Southern Derbyshire Clinical Commissioning Group
Improving the Quality of Care Provision for People at Risk of, or Who Have Had, Acute Kidney Injury in Derby Teaching Hospitals NHS Foundation Trust
The Trust has worked very closely with the CCG in developing and implementing quality improvement initiatives within the hospital. This close working and the senior buy in from the CCG has facilitated a pace of change within the hospital which has been supported by a CQUIN specific to acute kidney injury (AKI). The following describes the process and changes that have occurred. A further paper will follow which will share the impact of the changes in terms of outcomes for patients and use of health care resources.
The beginning
The national programme ‘Think Kidneys’ gave us the impetus to improve the quality of care related to AKI in Southern Derbyshire. The work to improve AKI related care within the hospital began following the first meeting of a steering group late 2013, which was convened by the CCG with key stakeholders from the Trust and other stakeholders. Representatives invited from the Trust included nephrologists, the head of medicine management, clinicians from acute medicine, cardiologists, pharmacists and patient safety and quality leads. As well from the CCG, the meeting was also attended by represented by patients, representatives from primary care, care homes and community pharmacy. This was seen as a unique and real opportunity for the Trust to work across the whole system and agreement was reached that the Trust would be involved in the development and implementation of AKI quality improvement initiatives. The steering group has continued to meet on a regular basis.
Development of the CQUIN
In January 2014 a draft CQUIN was developed for implementation in the contract with the Trust from April 2014. Nephrologists and quality leads from the Trust were able to contribute to the creation of the draft CQUIN. The opportunity to agree the detail within a CQUIN was a unique experience for the clinicians and resulted in a CQUIN that had full clinical support and was viewed as being clinically valuable and useful. As part of the CQUIN it was a requirement that the hospital should employ a project manager to co-ordinate the implementation of the CQUIN and ensure achievement of the desired outcomes.
The CQUIN was to have two parts – risk assessment and notification of AKI on discharge letters to primary care.
A. Risk Assessment
Development
Following the agreement of the CQUIN in January 2014, the team within the hospital were tasked with deciding which risk tool to implement and how to capture the outcome of the risk tool. The AKI risk assessment score developed in Grampian region was adopted and modified as in the pilot trial there were other comorbidities which were associated with the risk of AKI. It was important that the tool was easy to use and incorporated guidelines on what to do if risk was identified. Three actions were required if AKI risk was detected – U&Es daily, review medication and fluid balance assessment.
Implementation
Initially the results of the risk tool were captured on paper. This proved unsuccessful and results are now captured electronically. The input and co-operation of the IT department of the Trust was crucial and the success of the delivery of the CQUIN requirements was a direct result of having the hospital IT clinical lead as part of the team, and this was seen as a particular strength.
As part of the CQUIN a baseline was taken of completion of the risk tool and this baseline informed a trajectory for improvement in subsequent months of the CQUIN. The finance linked to the achievement of these incremental targets ensured the implementation of the risk tool remained a priority within the hospital. The actual baseline for completion of the risk tool was 60%, which was substantially higher than the expected 5 – 10%. To meet the incremental targets the IT system triggered an alert that the risk assessment had to be completed. To raise awareness the team also undertook various initiatives within the Hospital such as training junior doctors, pharmacists, highlighting AKI as a patient safety topic of the month, using AKI screen savers and patient stories. The risk tool was shared with the wider group of clinicians within the Trust as a tool that would help improve the care of their patients. The risk assessment score was initially analysed monthly and the score was revised by calculating the area under the curve (AUC) and determining the sensitivity and specificity.
Current performance as at June 2015 of completion of the risk assessment tool is 90%.
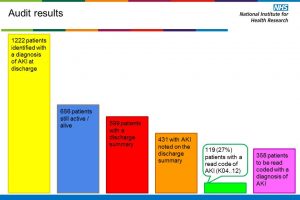
B. Discharge Summaries
The implementation of discharge summaries to include details of AKI detected during the hospital stay is the second part of the CQUIN. An early internal audit demonstrated that there was poor uptake due to the summary having to be completed manually. An IT solution has now been reached and standard wording for the three AKI levels, along with “no AKI” has been included in the IT system’s mandated discharge summary. Within this, free text is also possible. There were a number of issues to overcome prior to successful implementation of the electronic discharge summary. The standard wording within the discharge summaries have also been refined following feedback from GPs.
Current performance of completion of the discharge summary in June 2015 was 96.9%
Challenges
Below are the main challenges the team faced with the development and implementation of the risk tool and discharge summary:-
- Designing AKI risk assessment and mandated AKI diagnosis on discharge summary
- Development of interruptive alert for AKI risk assessment
- Development and changes to the IT system are time consuming
- Difficult to extract the codes to instigate a mandated discharge summary
- Time to analyse the data on regular basis
- Convincing wider clinical team of reason to undertake another task as part of their busy day
- Ensuring the message that the assessment was not the result expected but that the action required afterwards was the important result.
Why this was a success
Below are the things that enabled our achievements:-
- IT senior lead was a member of the team
- IT team were interested and keen to overcome the obstacles of implementation
- Excellent Trust Information department
- Senior buy-in from the CCG
- Project team chaired by CCG with representation from both hospital, CCG and community to cover the whole of the AKI pathway
- Clinical input into designing the CQUIN
- Resource from CQUIN to appoint a project manager within the hospital
- Linked funding to incremental targets within CQUIN
Contacts
If you would like further information about Derby Teaching Hospitals NHS Foundation Trust’s work on the care of patients with AKI and the development of the CQUIN please contact:-
- Nick Selby – Consultant Nephrologist – nick.selby@nhs.net
- Nitin Kolhe – Consultant Nephrologist nitin.kolhe@nhs.net
- Sandra Mir – Head of Patient Safety – sandra.mir1@nhs.net
Case studies