Case studies
The Establishment of an Acute Kidney Injury Service in a Tertiary Renal Centre at Lancashire Teaching Hospital NHS FT
Share this on – Facebook / Twitter / Linked In

Following an 18 month period of planning and confirmation of funding, an Acute Kidney Injury service at Lancashire Teaching Hospital NHS Foundation Trust was launched in October 2015. During the planning phase key stakeholders were identified and included in the service development. The renal directorate clinical director, the consultant nurse for critical care services, the critical care outreach team (CCOT), the renal pharmacist, the information technology (IT) department, the radiology department, the pathology and phlebotomy services, the quality and effectiveness lead for the organisation, the coding department, other specialist services such as the palliative care and pain team and the heart failure nurses. And finally to provide quality assurances, the Advancing Quality Alliance (AQuA) are involved as external reviewers. All stakeholders became key partners and had a significant impact on how the service was developed and implemented, especially the links with the IT and pathology department. This enabled us to develop robust processes to capture patient activity and documentation of Acute Kidney Injury Team (AKIT) interventions.
The AKIT is a bespoke service of the CCOT who, during the first 12 months of the service, spend approximately three months in the AKIT before rotating back into the CCOT. This period enables the individuals to develop additional skills and knowledge with this group of patients. The CCOT are now able to request renal ultrasound scans. Generating the service as an expansion of the CCOT was a deliberate decision taken to utilise the expertise and clinical knowledge of an established team of senior nurses familiar with assessing, planning, implementing and escalating the care of patients. The renal directorate practice educator joined the team, on a part time 12 month secondment to support service development, professional development of the existing CCOT. This resource has been invaluable to support the development of resources for ward-based education, and strengthen partnerships with the Renal Directorate.
The AKIT and the duty pharmacist identify their daily patient activity from a report on all AKI 1, 2 and 3 flags generated by a search on the organisation’s pathology system as per NICE guidance. The AKIT reviews all patients with AKI 2 and 3 every day, the ward based pharmacists review all AKI patients in their area Monday-Friday. The search is repeated frequently during the day to update in real time as blood tests are processed. One of the quality standards for patients with an AKI 3 is an early expert review. As the service operates 12 hours a day, 7 days a week, the majority of patients are reviewed within a 12 hour window following their blood results. The process for escalation of the patient with an acute kidney injury stage 3 mirrors that of the critical care outreach service but the AKIT escalates to the renal registrar or consultant on call. As the service has developed the need for timely blood samples has become evident so the appointment of additional phlebotomy services as part of the business case has been very useful. Good working relationships within the service facilitate daily discussion about patients to ensure best practice is implemented as soon as possible to achieve the best outcome, minimise patient deterioration and promote patient safety.
Recognition of acute kidney injury and appropriate coding at patient discharge is now included in the hospital discharge information letter and this has facilitated the funding stream to support the service in the longer term.
A large part of the AKIT’s responsibility is to provide education for all health care staff in all areas. Traditional teaching methods have been used, but release of staff from clinical areas is always challenging. 2
A short education session using ‘nearpod’ technology has been developed which can be delivered to ward staff in the clinical areas including health care support workers, nursing staff and medical teams. Established education sessions included in the organisation’s postgraduate training programme for nurses include AKI information, recognition and prevention. The team working with the renal consultants and pharmacists now have access to the foundation years medical educational programmes to deliver a joint session covering all the essential information. Contacts within primary care have facilitated access to GP training sessions held within the organisations health academy to deliver education on sepsis and AKI. One of the simplest tools to generate discussion about AKI is our team mascot ‘Sidney the Kidney’. Sidney engages staff in education sessions and information stands. He proved particularly popular at a local conference and was a talking point on the day. To support communication across our large teaching hospital the AKIT has developed a quarterly newsletter to raise awareness of the team and service in the organisation.
The AQuA AKI patient information leaflet has been adopted locally and is given to patients reviewed by the AKIT. Ongoing recommendations following patient discharge for GPs in relation to monitoring post AKI and patient information is also included in the hospital discharge letter for all stages of AKI, which support the AKI CQUIN measures.
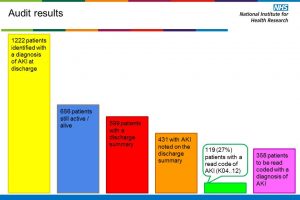
The organisation is working towards a ‘paper light’ vision by 2020. The AKIT future proofed their patient reviews by using the electronic patient record system to record the visit and brief interventions. The majority of information to support the AKI care bundle is recorded in the patient’s hard copy notes, not yet electronic until post discharge. This electronic record, at the time of the review, supports monitoring of AKIT activity and quality assurance for the organisation. Outcome measures and audit of the service run in line with the AQUA clinical process measures which are incorporated in the care bundle designed and used by the team. Monitoring and outcome measures will include numbers of patients seen by AKIT, numbers of visits per each patient group, numbers of patients requiring referral to CCOT and any changes to critical care outreach activity.
Specific outcome measures for AKI stage 3 will include length of hospital stay, mortality, percentage of hospital acquired compared to community, subsequent development of CKD and progression to dialysis. Specific outcome measures for AKI stage 2 include length of hospital stay, mortality, progression to AKI stage 3 and percentage of hospital acquired compared to that from the community.
In the future the service is planning the use of a blood order set for Vasculitis and point of care testing kits at the bed space. Within education we are exploring academic detailing for GPs, practice nurses and care homes and a learning placement for nursing and medical students. The team leader is working with a senior radiographer to promote the use of local hydration guidelines to minimise contrast media induced AKI. The lead renal physician is implementing a risk assessment to identify patients at risk of developing an AKI peri/post operatively who are attending pre-operative clinics.
The journey to date has been frustrating, challenging yet extremely rewarding. We have achieved the development of a robust quality driven acute kidney injury service for our patients, including the development of the knowledge and skill set of our critical care outreach team members which directly effects the service offered to our critically ill patients referred to the CCOT. The key rewards have been harvested by ensuring all stakeholders have been involved and their expertise have been utilised throughout service development. As the service matures we are constantly revisiting all elements to ensure we are satisfied with the service for our patients, this will create other ideas and potential developments to be considered.
Sally Fray, Critical Care Outreach Practitioner, Critical Care Outreach Team, Acute Kidney Injury Team, Lancashire Teaching Hospital NHS Foundation Trust
Case studies