Case studies
NIHR CLAHRC GM Case Study
Share this on – Facebook / Twitter / Linked In

This case study summarises the findings from the implementation and evaluation of the Sick Day Guidance project undertaken in NHS Salford Clinical Commissioning Group (CCG), in partnership with The National Institute for Health Research (NIHR) Collaboration for Leadership in Applied Health Research and Care (CLAHRC) Greater Manchester and Salford Royal NHS Foundation Trust (SRFT).
What were the reasons for the project?
Developing an evidence-based approach to address the harm associated with Acute Kidney Injury (AKI) is urgently warranted. Salford CCG embarked on a project to understand the implementation of sick day guidance cards to help prevent AKI in primary care.
The Salford CCG project was informed by work conducted in NHS Highland; which has led to medicine sick day guidance, for patients at risk of AKI, being made available nationally through the Scottish Patient Safety Programme. It was also informed by guidance from the National Institute for Health and Care Excellence and the Royal College of Physicians of Edinburgh, which recommend that temporary cessation of medicines should be considered during times of acute illness, for people at risk of AKI.
In England, the Think Kidneys Interim position statement on ‘sick day’ guidance highlights the potential benefits of providing sick day guidance as well as the potential harms. It states that ‘although there is strong professional consensus that advice on sick day guidance should be given, and this approach is advocated in the NICE AKI guideline, the evidence that provision of such advice reduces net harm is very weak.’ As such, position statement also indicates that ‘it is reasonable for clinicians to provide sick day rules,’ based on ‘individual risk assessment’, but recommends that widespread implementation should only be undertaken in the context a formal evaluation
It was in this wider context that Salford CCG collaborated with NIHR CLAHRC GM and SRFT to implement and evaluate sick day guidance cards for people at risk of AKI. The project ran between March 2015 and January 2016. Key objectives of the project included a need to understand factors surrounding the implementation of sick day guidance, with a view to provide a platform for a larger scale evaluation.
Who was involved?
Salford CCG based the cards on those used previously by NHS Highland. The project design was further developed with the Salford Partnership for Advancing Renal Care (SPARC) and NIHR CLAHRC Greater Manchester.
The project Steering Group* consisted of doctors, pharmacists and managers based at Salford CCG and SRFT, and research and project management staff from the NIHR CLAHRC Greater Manchester team.
What did the project entail?
The project had two strands: implementation (consisting of preventative interventions, supported by educational events) and a mixed methods evaluation.
Implementation
The project was launched in spring 2015 with educational events for multi-disciplinary healthcare teams, focussing on both raising awareness of AKI and the sick day guidance intervention. The project was conducted in the context of other kidney health initiatives being delivered across primary and secondary care in Salford. The intervention involved two main components:

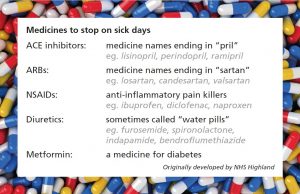
(i) Sick day guidance cards were provided to all 48 general practices and 60 community pharmacies for distribution to all patients who were taking any of the medicines listed on the card. An information leaflet was also provided to healthcare practitioners and administrators suggesting how to use and give the cards, although an overly prescriptive approach was avoided to allow health professionals to develop processes that worked best for individual patients. General practitioners were asked to record administration of the card to patients on practice systems, whereas community pharmacists were not. Support and resources were offered to general practices and pharmacies over three practice visits.
(ii) In three of the eight of the CCG neighbourhoods, practice pharmacists were employed to enhance medicines optimisation through several projects. Part of this work was to identify patients at risk of AKI who had been discharged from hospital and contacting those patients to discuss sick day guidance.
Evaluation
The evaluation took place during 2015-2016 and used mixed methods:
The Quantitative Evaluation
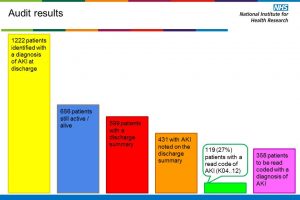
The aims of the quantitative research study were to ascertain activity levels and describe patient characteristics, using the Salford Integrated Record (SIR).
We analysed the Read code used for the administration of sick day guidance cards, and the patient characteristics. Analysis showed that coding was not recorded consistently. In view of this, analysis was limited to focusing on five general practices which were coding correctly. Within the five practices chosen, virtually all 1,452 eligible patients (with the exception of 2) were coded as receiving a card.
Results showed:
- 84% these of patients were hypertensive
- 35% had type 2 diabetes
- 20% were Read coded with a CKD stage between three and five
- One quarter of patients may have had a past episode of AKI (using the NHS England’s national AKI algorithm)
The Qualitative Evaluation
The qualitative evaluation explored the processes involved in implementing the intervention. We interviewed 24 clinicians and 5 patients, to explore their views. The interviews were recorded and analysed by the research team to organise content and identify themes.
- Sick day guidance cards were more readily integrated into existing long-term condition review appointments with practice nurses, as well as both ‘over the counter’ and medicine use reviews (MURs) carried out in community pharmacy.
- Practice-based pharmacists valued and engaged with the sick day project. However, they outlined numerous difficulties implementing the intervention including: being able to access patient data; more potentially relevant patients than anticipated; and fitting the work in with their pre-existing schedule.
- Communicating the concept of temporary cessation of medicines was a particular challenge to patient populations at higher risk of AKI.
- Health professionals struggled to ensure sick day guidance reach to all patient groups being prescribed the relevant medicines, particularly more vulnerable people e.g. those with reduced cognitive capacity.
Lessons Learnt
Feedback from the sick day guidance education sessions was positive, with participants’ self-reported AKI knowledge increasing.
Health practitioners have been having conversations with patients about AKI prevention; however, there are boundaries to the implementation of sick day guidance cards. Communicating the concept of temporary cessation of medicines was a particular challenge, in particular balancing the tension between reaching all required patients and achieving full patient understanding, especially when cognitive capacity was impaired. The qualitative data suggested that these conversations were more readily integrated into existing long-term condition review appointments with practice nurses and medicine use reviews (MURs) carried out in community pharmacy.
Evaluation of Phase Two of the intervention indicates that the integration of practice-based pharmacists into existing primary care teams is important to ensure data can be accessed and that pharmacists are able to focus their efforts on targeting the patients at highest risk of AKI.
Summary
Sick day guidance cards focussing solely on medicines management may be of limited benefit without either adequate resourcing, or if delivered as a standalone intervention. The development and evaluation of a range of primary care interventions, with a focus on patient health outcomes is needed to tackle the harm associated with AKI.
The full project report can be accessed from: http://clahrc-gm.nihr.ac.uk/our-work/kidney-health/salford-sick-day-guidance/.
*Steering Group Members
Rachel Airley (NIHR Clinical Research Network: Greater Manchester), Tom Blakeman (NIHR CLAHRC Greater Manchester), Rebecca Elvey (NIHR CLAHRC Greater Manchester), Jason Farrow (Salford CCG), Paolo Fraccaro (University of Manchester), Sam Glynn Atkins (NHS Salford CCG), Janet Hegarty (NIHR CLAHRC Greater Manchester, SRFT), Susan Howard (NIHR CLAHRC Greater Manchester), Liz Lamerton (SRFT), Anne-Marie Martindale (NIHR CLAHRC Greater Manchester), Aneela McAvoy (NIHR CLAHRC Greater Manchester), Sheila McCorkindale (Salford CCG), Rob Nipah (SRFT), Niels Peek (University of Manchester), Smeeta Sinha (SRFT), Claire Vaughan (Salford CCG), Sue Wood (NIHR CLAHRC Greater Manchester).
Case studies