Case studies
Improving Patient Safety and Reducing Harm through the Development of an Acute Kidney Injury Specialist Service at Wrightington, Wigan and Leigh NHS Foundation Trust
Share this on – Facebook / Twitter / Linked In

Overview
Acute Kidney Injury (AKI) is a life threatening condition that is common and harmful and in many cases avoidable, yet it can lead to 25% – 30% chance of mortality. AKI still very often appears to be an unfamiliar term within the healthcare profession and with the general public, highlighting the urgent need to raise the profile of AKI.
At Wrightington, Wigan and Leigh NHS Foundation Trust (WWL) our vision is “to be in the top 10% of hospitals for everything we do”, our mission is “to provide the best quality healthcare for all our patients”, our strategy is “to be safe, effective and caring” with patient safety always our highest priority of all, complying with the CQC inspection model. So this was at the forefront of setting up the AKI service.
WWL is a three site major acute trust providing the best possible healthcare for the people of Wigan, Leigh and surrounding areas. The trust has 758 inpatient beds in total covering 25 wards and is committed to designing services around the needs of our patients, and for patients to be cared for as close to their home as possible.
At WWL we have onsite renal department. Renal support is provided by our tertiary centre – Salford Royal NHS Foundation Trust. Their registrars provide 24/7 telephone advice and they transfer patients who require immediate renal specialist input in a timely manner. However, many patients do not require immediate transfer and the new AKI service provides close clinical input into the care of these patients to prevent deterioration and to optimise care. This is good both for the care of our patients and in alleviating the pressure on tertiary services / beds from District General Hospital referrals. We feel that the combination of a supportive tertiary centre and a locally focused AKI team has significantly improved care for patients with AKI.
National recognition of AKI as a significant a problem was the result of the NCEPOD report on the management of AKI in 2009. The NICE guidelines were then developed highlighting the importance of risk assessing and preventing AKI, early recognition and treatment and early referral to a specialist team. WWL put plans in place to develop the new AKI specialist service.
The AKI service was set up in 2014 with a consultant lead and a specialist nurse. We recognised the need to be responsive to people’s need and felt that this new service to treat and manage AKI was a definite requirement.
How the problem was analysed
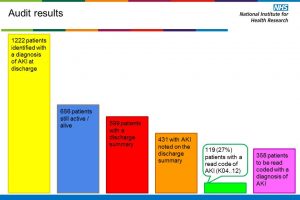
Recognising AKI as a national problem we carried out a baseline audit from August to December 2012 as part of the National NHS Kidney Care AKI Audit, looking at the management of patients diagnosed with a severe AKI, and also looking at morbidity and mortality.
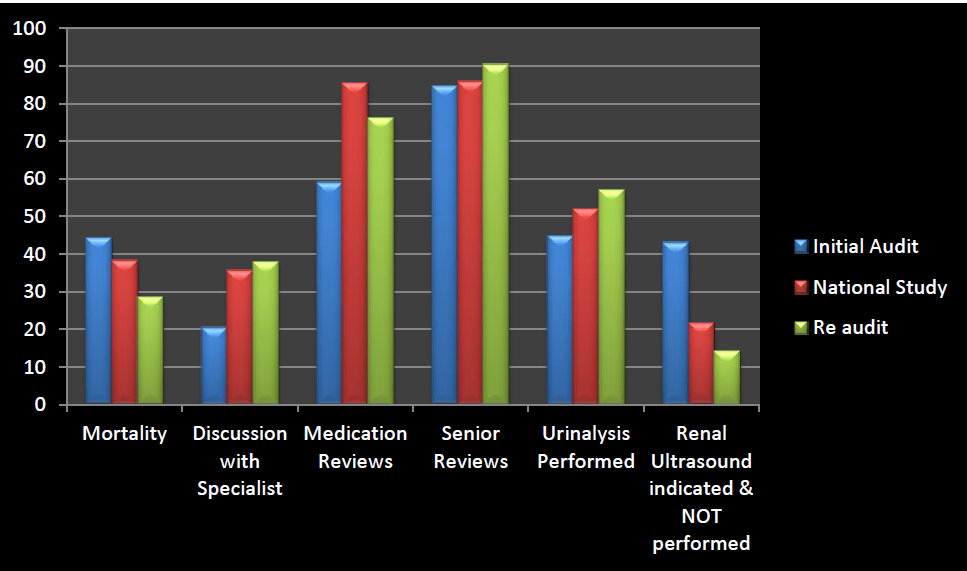
National results showed that WWL had higher mortality rates 1 month after severe AKI was diagnosed – our mortality was 44.2% compared to the study-wide average of 38.3%. It also showed we were performing poorly at medication reviews (59% compared to 85.5% study-wide) and for discussion with renal teams (20.5% compared to 35.7%).
In response to this a three month pilot was set up with the critical care outreach team to drive an AKI specific care bundle with excellent results which showed overall significantly reduced mortality.
We improved significantly in the following
- Number of ultrasound scans performed
- Medication reviews
- Discussions with renal team
- Senior reviews within 12 hours, and importantly
- Mortality was now lower than in the other 46 trusts in the national kidney audit.
The graph below shows the initial audit used for the National Kidney Care Audit, the national study results, and the re-audit showing the current practice since the AKI service was implemented in May 2014.
How we used a multi-disciplinary approach
Establishing awareness of the new service within the Trust was vital to ensure it would work, and education was the main priority. We developed a teaching programme to educate staff and raise awareness of AKI, and with this, the first stepping stone was in place to ensure successful establishment of the service.
We organised several drop-in sessions, and regular ward based teaching reached over 360 staff. An audit of pre and post knowledge of AKI showed promising results of improved knowledge after implementation of the teaching programme.
Through the recruitment of AKI ward champions we were able to distribute ward based learning and this helped staff on the wards to feel empowered.
Learning Opportunities
With the support of the incident reporting system – monthly safety thermometer, weekly audits of care which incorporate mortality reports and length of stay reports – we feel that our frontline staff are the prime people to identify problems and areas for improvement. Our staff are encouraged to report any incidents that occur.
The AKI service audits of care give us an excellent opportunity to target ward areas and carry out hands-on ward based training on a one to one basis enabling reflection of events which are considered learning opportunities.
Evidence that the AKI Service has improved safety and reduced harm and is sustainable
Since the implementation of the AKI service over the last 12 months we have achieved many sustainable improvements, these include:
- Development of the AKI Care Bundle
- Production of a patient education leaflet
- Introduction of telephone follow up calls
- Analysis of patient experience questionnaires
- Implementation of the AKI e-alert system as per the national algorithm and the NHS England Patient Safety Alert in June 2014
- Development and delivery of the AKI education programme
- Identification and skills development of AKI Ward Champions
- Creation of a service that offers advice and support to all clinical staff caring for those diagnosed with an AKI.
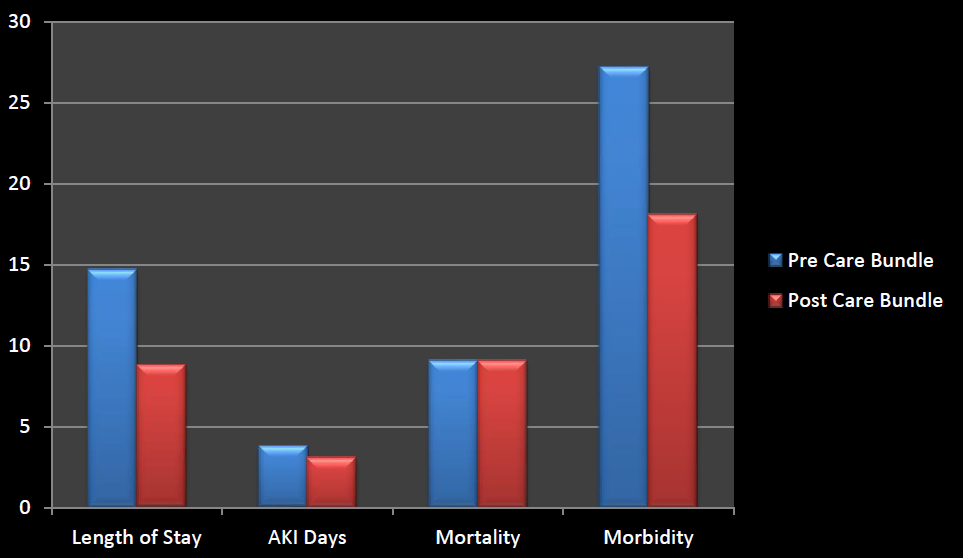
The first 24 hours of treatment is fundamental for AKI patients to recover without significant consequences to normal renal function, and to prevent deterioration or the need for escalation to a higher area of care. To facilitate the integral, timely care of AKI patients, a new re-evaluated and re-invigorated AKI Care Bundle, in accordance with NICE CG 169, has now been distributed to each ward area. This includes step by step criteria for the first 24 hours of treatment for all stages of AKI and the re-audit data shows:
- Improved length of stay:
- pre AKI care bundle LOS 14.7 days and average number of AKI days 3.8
- following introduction of the AKI care bundle average LOS has reduced to 8.8 days and the average number of AKI days is down to 3.1
- Improved morbidity
- A reduction in number of Stage 3 AKI patients
As part of improving early recognition of AKI we now have AKI alerts on the EPR system that highlight the stage of AKI at the bottom of blood test results. This enables definite diagnosis of AKI to be recognised against the national algorithm, and the patient is then treated accordingly.
Patient engagement
Patient and carer education about AKI is equally important. In order to support this a patient education leaflet has been created and is shared with every patient diagnosed with AKI. The leaflet describes what AKI is and how to prevent it occurring again. It also provides discharge advice and incorporates sick day rules to help prevent AKI occurring in the community.
The new service also provides a telephone follow up service. Anecdotal evidence is showing that patients are very appreciative of this service and find comfort in the follow up.
Patient experience questionnaires are demonstrating to us how beneficial the service within the Trust is and how patients feel that their overall experience from the AKI service perspective is positive and reassuring.
How best practice was identified and built on
The AKI Specialist Service is a brand new service nationally with not many acute trusts currently offering the service. We believe that we are the first District General Hospital to be fortunate enough to have such a service and have been guided by the NICE Guideline for caring for AKI patients from diagnosis to renal replacement therapy.
We have been contacted by many trusts in the country about our new service and some have come to work and learn alongside us as they develop the AKI service within their trust.
We are now looking to expand the team to enable follow up clinics to take place and reach out to primary care with in-house education for GP practice nurses and nursing home staff.
Conclusion
The new AKI Service has exceeded expectations and is above and beyond what WWL NHS FT had in place originally. The AKI service is well-established and effective and receives many referrals to see patients. Having a point of contact and face to face consultation has proved beneficial to both patients/families as well as clinical staff.
The AKI service has given clinical staff an increased awareness of AKI through face to face teaching sessions held regularly within the Trust, and this increased awareness in turn generates a culture of improved and timely treatment of AKI. Having a daily ward presence of an AKI Specialist Team is extremely beneficial, continually promoting awareness of the service and of AKI.
We have been asked to present to other trusts how the service was set up, the benefits of an AKI Specialist Service and the achievements and positive results from data that have been accomplished.
Dramatically reducing mortality rates, length of stay, the number of AKI days since the implementation of the service, as well as the number of patients being diagnosed with AKI, are great achievements for our Trust and deliver what we most want – improved outcomes and safety for our patients.
Dr Stephen R Gulliford FRCP, Consultant – Acute Medicine Clinical Director and Suzanne Wilson, Acute Kidney Injury Specialist Nurse
Case studies