Case studies
Acute Kidney Injury in the Oncology Population – A Novel Quality Improvement Initiative
Share this on – Facebook / Twitter / Linked In

This case study has been written by Tamer Al-Sayed, Consultant in Acute & Renal Medicine, University Teaching Hospital of South Manchester NHS Foundation Trust, working with Gerry Campbell, Acute Oncology Advanced Nurse Practitioner, The Christie NHS Foundation Trust, who are pictured here.
If you would like to contact Tam about this work, please email tamalsayed@doctors.org.uk
Recognising the need
In October 2014, a novel collaboration between The University Teaching Hospital of South Manchester NHS Foundation Trust and The Christie Hospital NHS Foundation Trust was established. This joint venture was the first of its kind in the United Kingdom, meaning that for the first time a tertiary stand- alone cancer centre would benefit from on-site daily senior decision makers at the front door.
From its very inception this unique model of working presented us with a golden opportunity to undertake work on AKI that had previously not been considered. My nephrology background meant that I was able to realise that there was an unmet need for AKI recognition, prevention and management. The driver for change was the NICE guidance, NCEPOD report on AKI and emerging worldwide literature in this new evolving sub-speciality of ‘Onco-Nephrology’.
Who we are
In order to realise our goals a working group was established, chaired by our deputy medical director and clinically steered by myself. There was broad participation on this group including:
- Acute oncology advanced nurse practitioner
- Acute oncology outreach nurse practitioner
- Consultant haematologist
- Consultant chemical pathologist
- Consultant radiologist
- Lead CT radiographer
- Clinical audit lead
- Medical informatics
- Clinical director of pharmacy services
- Change was affected by means of strong clinical and executive leadership that inspired the team to disseminate our objectives to their colleagues and respective clinical teams. In the last 18 months there has been a clearly observable shift in culture with adoption of this work across the trust.
What we did
To date we have been successful in progressing the following pieces of work:
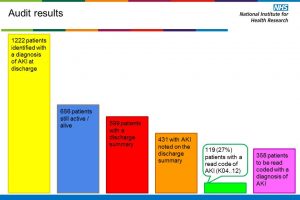
- Quantifying the burden of AKI in our acute oncology admissions receiving systemic anti-cancer therapy (SACT) by utilising AKI e-alerts
- Developing a front door risk recognition tool and care bundle to enable prompt management of high risk patients diagnosed with AKI
- Implementing a hotline triage tool for patients with diarrhoea & vomiting
- Establishing a robust medicines optimisation process for ensuring prompt discontinuation of medication that can cause renal perturbations in the acute setting
- Trialling new fluid balance/urinalysis charts on our oncology assessment unit (OAU)
- Introducing a trust wide AKI guidance as part of our online acute oncology emergency handbook that includes a patient information leaflet
- Providing regular AKI education through various forums for nurses and doctors
- Consolidating on our established contrast induced nephropathy guidance in CT with the radiology department
- Presenting our work and data locally, regionally and nationally
- Patient safety award nomination
What next?
Going forward we are in the process of delivering the following pieces of vital work:
- Displaying AKI dashboards on all oncology wards
- Incorporating AKI tools onto our clinical web portal, e-records and e-prescribing
- Developing e-learning bytes for all clinical staff
- Publishing our long term data
- Undertaking biomarker assay studies for risk stratification purposes
Lessons we’ve learned along the way
- Utilising a simple risk recognition tool and management care bundle
- Ensuring regular updates of progress to departmental clinical directors
- Earlier IT & business intelligence involvement
- Defining generic aims at the outset and then refining them to study individual disease groups
Case studies